A 28-year-old man was admitted to our hospital with worsening, ulcerating skin lesions on his face, arms and trunk. Six months prior, he had been diagnosed with HIV infection and hospitalized with Pneumocystis jiroveci pneumonia for which he received treatment with trimethoprim-sulfamethoxazole (TMP/SMX). Three intramuscular doses of penicillin benzathine were also administered for a positive RPR (titer 1:32).
Five months later, he was started on a highly active antiretroviral therapy (HAART) regimen, including emtricitabine, tenofovir, atazanavir, and ritonavir. Soon after, the patient noticed painless, non-pruritic, reddish nodules, initially on his face, later on his arms. A seven-day course of oral clindamycin had no effect. Instead, additional lesions appeared over his trunk and extremities and the facial lesions progressed in size, and ulcerated. In addition, he complained of fatigue, a dry cough and diffuse arthralgias. He denied travel, recent sick contacts, intravenous drug use, outdoor activities or animal exposures.
He identified himself as being homosexual and lived in an urban setting in the Northeast of the United States.
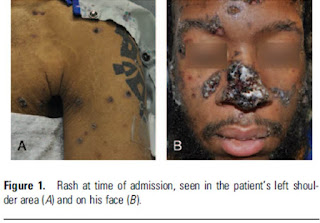
On examination, the patient was in no distress, afebrile, normotensive, but tachycardic with a pulse rate of 127 beats/minutes. Scattered skin lesions, varying in size from 0.5 to 5 cm were present. Some were nodular and intact (Figure 1A); larger ones were ulcerated and/or crusted (Figure 1B). No mucosal involvement or adenopathy were noted. His right knee was moderately swollen without warmth, erythema or tenderness.
Routine laboratory testing revealed anemia, mild hyponatremia and mild hyperbilirubinemia. The RPR titer was unchanged. Blood cultures were obtained. His CD4 cell count had increased from 64 to 72 cells/mm3 (11% to 40%) and his HIV viral load had fallen one log from 214 570 to 19 009 copies/mL since initiation of HAART. A chest radiograph revealed scattered patchy opacities without effusions. Arthrocentesis of the right knee yielded 896 red blood cells/mm3 and 3380 white
blood cells/mm3 (88% neutrophils); fluid cultures were sent. A biopsy of the facial skin lesions was performed (Figure 2).
What diagnosis best explains the patient’s progressive skin lesions?
Clinical Infectious Diseases 2013;56(1):117
















.png)






0 comentarios:
Dí lo que piensas...